Ill. Imaging Findings of COVID-19 Patients
Thoracic imaging is of great value in the diagnosis of C0VID-19, monitoring of therapeutic
efficacy, and patient discharge assessment. A high-resolution CT is highly preferable. Portable
chest X-rays are helpful for critically ill patients who are immobile. CT for baseline evaluation
of patients with C0VID-19 is usually performed on the day of admission, or if ideal therapeutic
efficacy is not reached, it can be re-performed after 2 to 3 days. If symptoms are stable or
improved after treatment, the chest CT scan can be reviewed after 5 to 7 days. Daily routine
portable chest X-rays are recommended for critically ill patients.
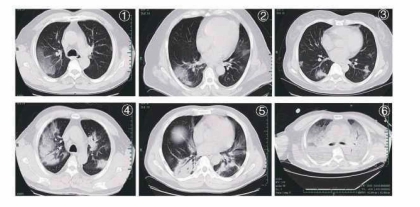
C0VID-19 at the early stage often presents with multifocal patchy shadows or ground glass
opacities located in the lung periphery, subpleural area, and both lower lobes on chest CT
scans. The long axis of the lesion is mostly parallel to the pleura. Interlobular septa I thickening
and intralobular interstitial thickening, displaying as subpleural reticulation namely a "crazy
paving" pattern, is observed in some ground glass opacities. A small number of cases may
show solitary, local lesions, or nodular/ patchy lesion distributed consistent with bronchus
with peripheral ground glass opacities changes. Disease progression mostly occurs in the
course of 7-10 days, with enlarged and increased density of the lesions compared with
previous images, and consolidated lesions with air bronchogram sign. Critical cases may show
further expanded consolidation, with the whole lung density showing increased opacity,
sometimes known as a "white lung". After the condition is relieved, the ground glass opacities
can be completely absorbed, and some consolidation lesions will leave fibrotic stripes or
subpleural reticulation. Patients with multiple lobular involvement, especially those with
expanded lesions should be observed for disease exacerbation. Those with typical CT pulmo�
nary manifestations should be isolated and undergo continuous nucleic acid tests even if the
nucleic acid test of SAR-CoV-2 is negative.
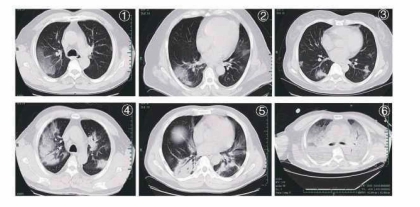
Typical CT features of C0VID-19 :
Figure 1, Figure 2: patchy ground glass opacities;
Figure 3: nodules and patchy exudation;
Figure 4, Figure 5: multifocal consolidation lesions;
Figure 6: diffuse consolidation, "white lung''.
IV. Application of Bronchoscopy in the Diagnosis and
Management of COVID-19 Patients
Flexible bronchoscopy is versatile, easy to use, and well tolerated in mechanically ventilated
COVID-19 patients. Its applications include:
(1) Collection of respiratory specimens from the lower respiratory tract (i.e. sputum,
endotracheal aspirate, bronchoalveolar lavage) for SARS-CoV-2 or other pathogens guides
the selection of appropriate antimicrobials, which may lead to clinical benefits. Our experi�
ence indicates that lower respiratory specimens are more likely to be positive for SAR-CoV-2
than upper respiratory specimens.
(2) Can be used for localization of the site of bleeding, cessation of hemoptysis, sputum or
blood clots removal; if the site of bleeding is identified by bronchoscopy, local injection of
cold saline, epinephrine, vasopressin, or fibrin as well as laser treatment can be performed
via the bronchoscope.
(3) Assist in the establishment of artificial airways; guide tracheal intubation or percutane�
ous tracheotomy.
(4) Drugs such as infusion of a-interferon and N-acetylcysteine can be administrated via the
bronchoscope.
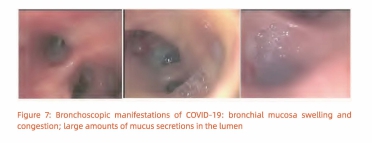
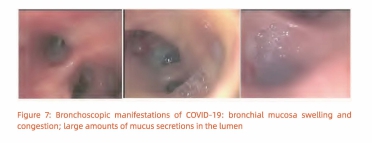
Bronchoscopic views of extensive bronchial mucosa[ hyperemia, swelling, mucus-like
secretions in the lumen and jelly-like sputum blocking the airway in critically ill patients.
(Figure 7)
V. Diagnosis and Clinical Classification of COVID-19
Early diagnosis, treatment and isolation should be carried out whenever possible. Dynamic
monitoring of lung imaging, oxygenation index and cytokine levels are helpful for early
identification of patients who may develop into severe and critical cases. A positive result of
the nucleic acid of SARS-CoV-2 is the gold standard for the diagnosis of COVID-19. However,
considering the possibility of false negatives in nucleic acid detection, suspected cases
characteristic manifestations in CT scans can be treated as confirmed cases even if the nucleic
acid test is negative. Isolation and continuous tests of multiple specimens should be carried
out in such cases.
The diagnostic criteria follow Protocols for the Diagnosis and Treatment of CDVID-2019. A
confirmed case is based on epidemiological history (including cluster transmission), clinical
manifestations (fever and respiratory symptoms), lung imaging, and results of SARS-CoV-2
nucleic acid detection and serum-specific antibodies.
Clinical Classifications:
Mild Cases
The clinical symptoms are mild and no pneumonia manifestations can be found in
imaging.
Moderate Cases
Patients have symptoms such as fever and respiratory tract symptoms, etc. and
pneumonia
manifestations can be seen in imaging.
Severe Cases
Adults who meet any of the following criteria: respiratory rate ;;, 30 breaths/min;
oxygen saturations; 93% at a rest state; arterial partial pressure of oxygen (PaO,)/oxy�
gen concentration (FiO,) s; 300 mm Hg. Patients with> 50% lesions progression within 24
to 48 hours in lung imaging should be treated as severe cases.
Critical Cases
Meeting any of the following criteria: occurrence of respiratory failure requiring
mechanical ventilation; presence of shock; other organ failure that requires monitoring
and treatment in the ICU.
Critical cases are further divided into early, middle and late stages according to the
oxygenation index and compliance of respiratory system.
• Early stage: 100 mmHg <oxygenation index s;lSO mm Hg; compliance of respiratory
system ;;,30 ml/ cmH,O; without organ failure other than the lungs. The patient has a
great chance of recovery through active antiviral, anti-cytokine storm, and supportive
treatment.
• Middle stage: 60 mmHg < oxygenation index s;lOO mmHg; 30 mL/cmH,O >
compliance of respiratory system ;;el 5 mL/cmH,O; may be complicated by other mild or
moderate dysfunction of other organs.
• Late stage: oxygenation index s; 60 mmHg; compliance of respiratory system <15
mL/cmH,O; diffuse consolidation of both lungs that requires the use of ECMO; or failure
of other vital organs. The mortality risk is significantly increased.